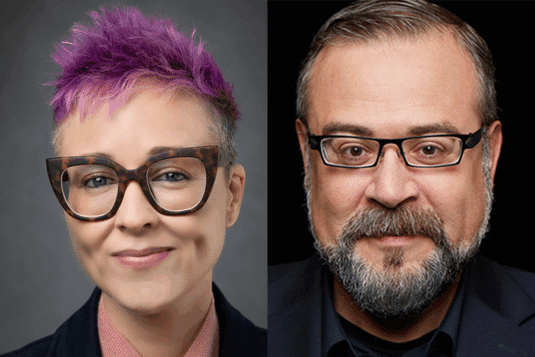
Cait DesRoches and Liz Salmi reflect on the evolution of open notes and issue a clear call to action for oncology. Drawing on over fifteen years of research, they underscore that while open notes consistently strengthen trust, understanding, and patient engagement, access is not equitable. They argue that transparency without equity is incomplete.
Ethics
Critical AI Health Literacy as Liberation Technology: A New Skill for Patient Empowerment
As artificial intelligence transforms health care, patients are increasingly using generative AI to question, reinterpret, and even resist institutional decisions. This provocative commentary, from Hugo Campos and Liz Salmi, introduces “Critical AI Health Literacy” as a new skill set for patients seeking agency and equity in the digital age of medicine.
Near-wins in the pursuit of quality: does transparency matter if no one is looking?
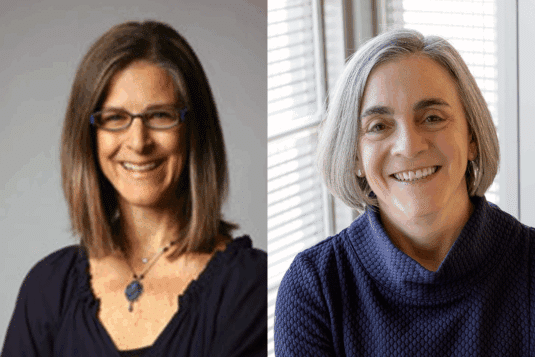
In this new editorial for BMJ Quality & Safety, Sigall Bell, MD and Cait DesRoches, DrPH reflect on how access to medical notes can improve the quality of care, but only if patients are able to read and understand them. In the time between medical visits, when patients are monitoring their own health, AI may open a new frontier.
Patient portals fail to collect structured information about who else is involved in a person’s care
“Shared access” uses separate identity credentials to differentiate between patients and care partner portal users. EHR vendors must recognize that both patients and care partners are important users of their products and acknowledge and support the critical contributions of care partners as distinct from patients.
21st Century Cures Act ONC Rule: Implications for adolescent care and confidentiality protections
This article reviews the key aspects of confidentiality protections in adolescent health care, explains the ONC Rule, outlines clinical, HIT, and equity challenges associated with its implementation, encourages the development of policies protecting the confidentiality of adolescents’ EHI [ … ] and offers tools for analyzing key questions in individual cases and practical steps to address the confidentiality of EHI with patients and parents.
Clinical ethics consultation documentation in the era of open notes
The new regulatory requirements of the 21st Century Cures Act provide a valuable opportunity to involve patients more actively in the documentation and telling of their own story of ethical complexity. Healthcare systems should take advantage of this new era and use open notes as a way to improve CECs documentation and, ultimately, patient care.
Open notes in patient care: confining deceptive placebos to the past?
In some countries, the practice of “open notes” is advanced with patients using online portals to access their clinical records. In this report, the authors reflect on the consequences of access for placebo prescribing, particularly for the common practice of deceptive placebo use, in which patients are not aware they are being offered a placebo.
We need to talk about “closed notes”
In this personal blog, the author discusses the harmful consequence of “closed notes” – of denying patients rapid access to their online clinical information. The blog post describes “closed notes” as an inherited structure in healthcare but urges that this does not make it right.
OpenNotes: Anticipatory Guidance and Ethical Considerations for Pediatric Psychologists in Interprofessional Settings
The OpenNotes era has ushered in the possibilities of greater patient and family collaboration in shared decision-making and reduced barriers to documentation sharing. However, it has raised new ethical and clinician documentation considerations. In addition to clinician education, patients and families could benefit from education around the purpose of clinical documentation, how to utilize OpenNotes, and the benefits of engaging in dialogue regarding the content and tone of documentation.
Patients, clinicians and open notes: information blocking as a case of epistemic injustice
We address the contrasting perceptions of this practice innovation, and claim that the divergent views of patients and clinicians can be explained as a case of epistemic injustice. Using a range of evidence, we argue that patients are vulnerable to (oftentimes, non-intentional) epistemic injustice. Nonetheless, we conclude that the marginalisation of patients’ access to their health information exemplifies a form of epistemic exclusion, one with practical and ethical consequences including for patient safety.