Patient portal use among patients with cancer has increased significantly in recent years. This state-of-the-art review seeks to address and analyse literature involving patient portal use by patients with cancer and their care partners.
Proxy Access/Caregivers
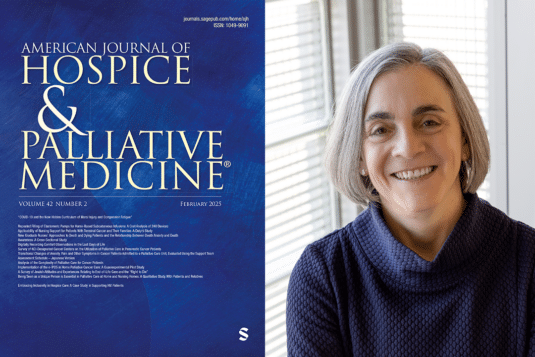
Is Routine Discharge Enough? Needs and Perceptions Regarding Discharge and Readmission of Palliative Care Patients and Caregivers
This study investigated the hospital discharge process for palliative care patients and their caregivers, focusing on its patient-centeredness, discharge readiness, and links to readmissions.
Shared access to adults’ patient portals: A secret shopper exercise
Our secret shopper exercise unveiled noteworthy variability in the experiences of 18 individuals attempting to grant or receive shared access to the patient portal, highlighting multiple barriers and facilitators to shared access. The findings underscore the imperative for cross- and intra-organizational collaboration aimed at learning from the diverse experiences of patients, care partners, clinicians, and staff, and disseminating best practices.
Identifying research priorities and essential elements of palliative care services for people facing malignant brain tumors: A participatory co-design approach
Malignant brain tumors (brain cancer) significantly affects the quality of life (QoL) of patients and their care partners, particularly in areas like cognition and communication. This study aimed to find out the top research priorities for palliative care in brain cancer using a collaborative, community-driven approach.
Patient portals fail to collect structured information about who else is involved in a person’s care
“Shared access” uses separate identity credentials to differentiate between patients and care partner portal users. EHR vendors must recognize that both patients and care partners are important users of their products and acknowledge and support the critical contributions of care partners as distinct from patients.
Pediatric open notes: Caregiver experiences since the 21st century Cures Act
While research on the impact of Open Notes in pediatric inpatient settings remains limited, recent findings have improved our understanding by adding actual caregiver experiences to the expectations identified in our initial study. As we move into this new era of transparency, we call for further investigation of the impact of note sharing on health care outcomes for children while continuing to develop strategies to mitigate challenges.
Co-designing an initiative to increase shared access to older adults’ patient portals: Stakeholder engagement
We partnered with 3 health care organizations to co-design an initiative that aimed to increase shared access registration and use and that can be implemented using existing patient portals. Educational materials are publicly available at Coalition for Care Partners.
Catalyzing dementia care through the learning health system and consumer health information technology
This perspective discusses how emerging payment models, quality improvement initiatives, and population health strategies present opportunities to embed best practice principles of ADRD care within the LHS. We aim to stimulate progress toward sustainable infrastructure paired with person- and family-facing innovations that catalyze broader transformation of ADRD care.
Shared access to patient portals for older adults: Implications for privacy and digital health equity
This viewpoint article discusses challenges and opportunities of systematic engagement of care partners through shared access to the patient portal that have been amplified in the context of the COVID-19 outbreak and recent implementation of federal information blocking rules to promote information transparency alongside broader shifts toward care delivery innovation and population aging. We describe implementation considerations and the promise of granular, role-based privacy controls in addressing the nuanced and dynamic nature of individual information sharing preferences and fostering person- and family-centered care delivery.
The Value of OpenNotes for Pediatric Patients, Their Families and Impact on the Patient–Physician Relationship
Although limited by relatively low survey response rate, OpenNotes was well-received by parents of pediatric patients without untoward consequences. The main concerns pediatricians raise about OpenNotes proved to not be issues in the pediatric population. Our results demonstrate clear benefits to adoption of OpenNotes. This provides reassurance that the transition to sharing notes with pediatric patients can be successful and value additive.